If you’ve ever gone down the rabbit hole of fungal acne advice online, you’ve probably seen this claim:
“Avoid all fatty acids between C12 and C24—they feed Malassezia, the yeast that causes fungal acne.”
It sounds scientific. It references chain lengths and biochemistry. But is it the whole truth?
Not quite.
Like many viral skincare “facts,” this claim is based on a grain of science that’s been taken out of context. Today, we’re going to break down what research really says about lipids, fungal acne, and whether you need to ditch your favourite moisturiser just because it has a fatty acid in it.
Let’s Start with the Basics: What Is Fungal Acne?
Fungal acne is the nickname for a condition called Malassezia folliculitis—an overgrowth of yeast (especially Malassezia furfur) in your hair follicles. Unlike bacterial acne, it doesn’t respond to benzoyl peroxide or antibiotics. Instead, it often shows up as itchy, uniform pustules, especially on the forehead, chest, and back.
Seborrheic dermatitis is another skin condition where Malassezia is a primary culprit. This chronic inflammatory disorder typically presents as flaky, greasy scales, redness, and itching, commonly in areas with high sebum production like the scalp, eyebrows, and sides of the nose. Clinical and microbiological studies have confirmed that Malassezia species trigger inflammation by metabolising sebum lipids into irritants such as oleic acid, which disrupts the skin barrier and induces cytokine release.
Where the Fatty Acid Fear Started
The origin of the "no C12–C24 fatty acids" rule comes from in vitro (lab-based) studies. Researchers like DeAngelis et al. (2005) cultured Malassezia in petri dishes and found that it couldn’t grow unless certain fatty acids were present, particularly medium- and long-chain fatty acids ranging from 11 to 24 carbon atoms in length.
This is true—in a test tube.
But here's the thing: your skin is not a petri dish. Real skin is a living ecosystem with a microbiome, immune defences, and a complex barrier system. What feeds yeast in a lab doesn’t necessarily feed it on your face.
Real Skin ≠ Petri Dish
Malassezia doesn’t just grow because a lipid is present. It depends on:
-
The lipid’s availability in free form
-
Skin pH
-
Presence of competing microbes
-
Sebum composition
-
Immune status of the skin (e.g., IL-17 levels, AMP production)
In real life:
-
Many problematic fatty acids are already present in sebum (e.g., oleic acid, palmitic acid).
-
Skincare lipids like cholesteryl esters, ceramides, hydrogenated lecithin are not metabolized the same way.
-
Some lipids can’t penetrate to where Malassezia resides (inside follicles) and have no real-world impact on yeast proliferation.
The Real World Tells a Different Story
In actual clinical research—on real people, not yeast in a dish—the story changes.
1. Lipid-Rich Creams Can Actually Improve Fungal Acne Symptoms
In one clinical study, a cream containing phytosphingosine, a lipid with an 18-carbon tail, reduced symptoms of seborrheic dermatitis (a related Malassezia-driven condition) in patients. This is despite the fact that phytosphingosine falls within the dreaded C12–C24 range.
2. Barrier Repair Matters More Than Fatty Acid Length
In another study, Sugarman et al. (2005) showed that ceramide-dominant barrier creams, rich in lipids like cholesterol and fatty acids, helped improve atopic skin and did not worsen fungal conditions. Lipids like ceramides and cholesterol are structured in a way that Malassezia can’t easily use as food.
3. Lipid Starvation Backfires
Avoiding all lipids out of fear can actually weaken your skin barrier, making you more prone to irritation, inflammation, and yes, even more breakouts. Lipids like squalane, ceramides, hydrogenated lecithin, and phytosterols are essential for healing and resilience and don’t feed Malassezia.
So Why the Confusion?
Online lists of "Malassezia-safe ingredients" are often based on ingredient isolation, not formulation science. They don’t account for:
-
Whether the fatty acid is free or esterified
-
Whether it’s bioavailable in a formula
-
How deeply it penetrates into the hair follicle
-
The presence of antifungal actives that offset lipid content
-
The skin’s immune regulation, pH, and microbial competition
For example, glyceryl stearate contains stearic acid (C18), but it's not the same as applying free stearic acid. It's part of an emulsifier complex that doesn’t release the fatty acid in a usable form for yeast.
Bottom Line
The internet often overcorrects. While it’s true that Malassezia can metabolise certain fatty acids in vitro, this doesn’t mean you must avoid every lipid between C12 and C24. Skin is smarter than that, and so should your skincare strategy.
Formulation, delivery, and context matter. Barrier repair is not optional...it’s foundational. When done right, it doesn’t feed fungal acne; it helps eliminate it.
Read more
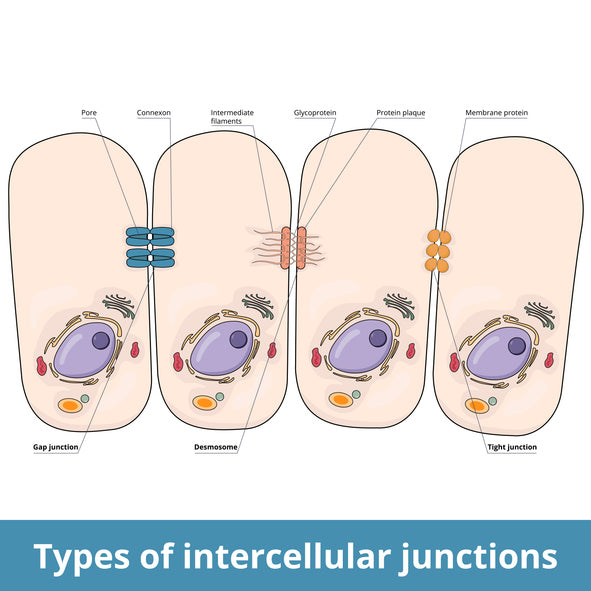
Your Skin Barrier Is Smarter Than You Think .....And Its Survival Starts With DesmosomesMost skincare conversations stop at hydration and collagen. But emerging research shows the real guardians of...
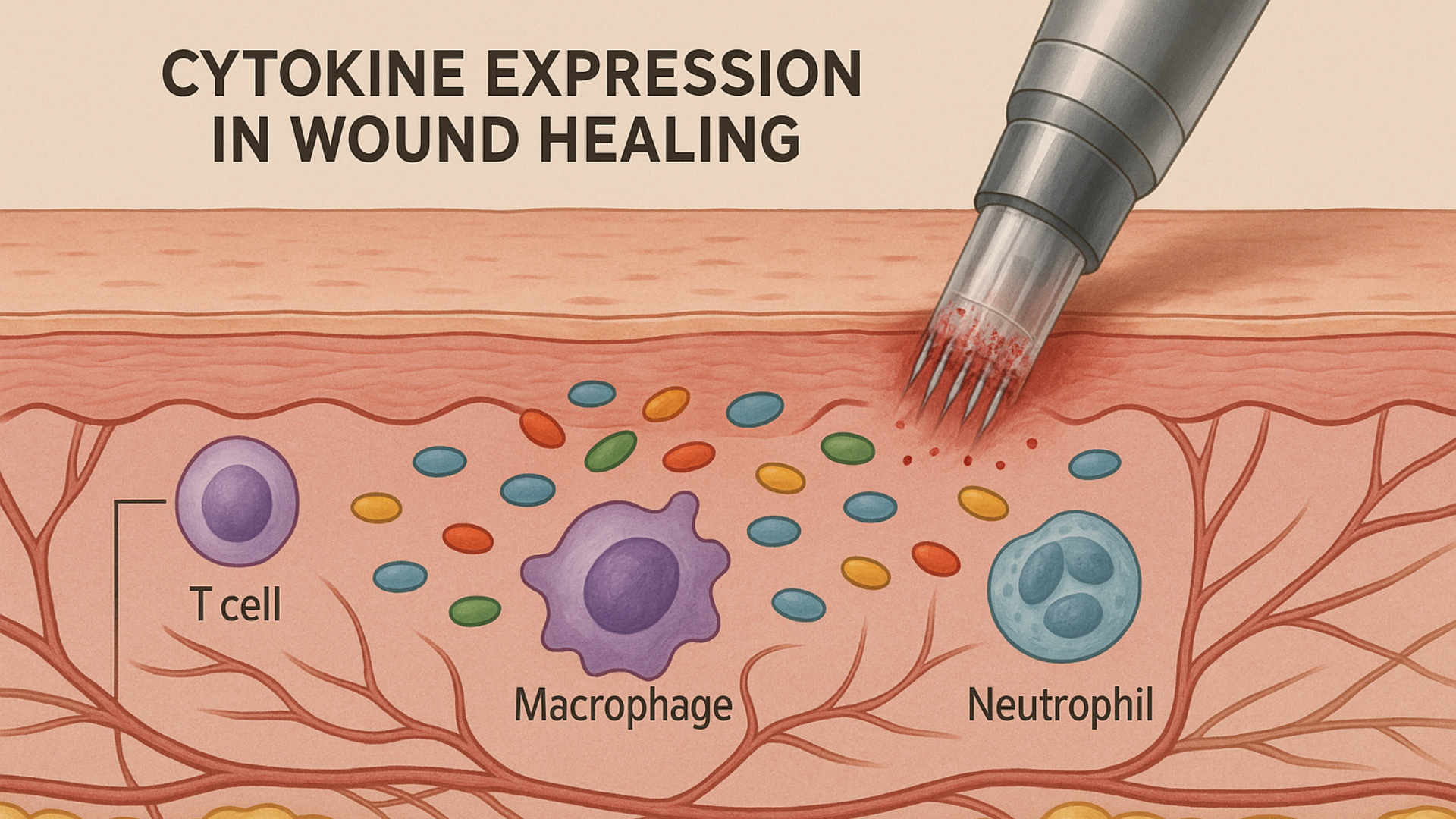
What Microneedling Can Teach Us About Interpreting Cosmetic Science Properly Nothing grinds my gears more than misinformation being sprouted as science, especially when it comes from those who thin...



